2022-06-29

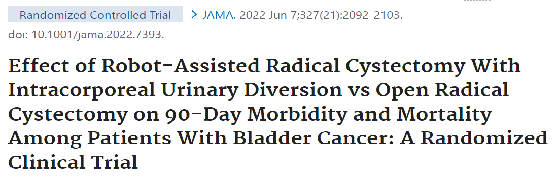
Catto JWF, JAMA. 2022 Jun 7;327(21):2092-2103.
机器人辅助根治性膀胱切除术的频率越来越高,但与膀胱癌开腹根治性膀胱切除术相比,全体内手术是否能提高康复率尚不清楚。目的比较机器人辅助根治性膀胱切除术与体内重建与开腹根治性膀胱切除术后的恢复和发病率
2017年3月至 2020年3月在英国9个地点招募的非转移性膀胱癌患者的随机临床试验。随访时间分别为90天、6个月和12个月,最终随访时间为2021年9月23日。参与者被随机分配接受机器人辅助根治性膀胱切除术和体内重建(n = 169)或开放根治性膀胱切除术(n=169)
在接受根治性膀胱切除术的非转移性膀胱癌患者中,机器人辅助根治性膀胱切除术联合体外尿流改道与开放性根治性膀胱切除术相比,90 天内的存活天数和出院天数显着增加。然而,这些发现的临床重要性仍不确定。
Abstract
Importance: Robot-assisted radical cystectomy is being performed with increasing frequency, but it is unclear whether total intracorporeal surgery improves recovery compared with open radical cystectomy for bladder cancer.
Objectives: To compare recovery and morbidity after robot-assisted radical cystectomy with intracorporeal reconstruction vs open radical cystectomy.
Design, setting, and participants: Randomized clinical trial of patients with nonmetastatic bladder cancer recruited at 9 sites in the UK, from March 2017-March 2020. Follow-up was conducted at 90 days, 6 months, and 12 months, with final follow-up on September 23, 2021.
Interventions: Participants were randomized to receive robot-assisted radical cystectomy with intracorporeal reconstruction (n = 169) or open radical cystectomy (n = 169).
Main outcomes and measures: The primary outcome was the number of days alive and out of the hospital within 90 days of surgery. There were 20 secondary outcomes, including complications, quality of life, disability, stamina, activity levels, and survival. Analyses were adjusted for the type of diversion and center.
Results: Among 338 randomized participants, 317 underwent radical cystectomy (mean age, 69 years; 67 women [21%]; 107 [34%] received neoadjuvant chemotherapy; 282 [89%] underwent ileal conduit reconstruction); the primary outcome was analyzed in 305 (96%). The median number of days alive and out of the hospital within 90 days of surgery was 82 (IQR, 76-84) for patients undergoing robotic surgery vs 80 (IQR, 72-83) for open surgery (adjusted difference, 2.2 days [95% CI, 0.50-3.85]; P = .01). Thromboembolic complications (1.9% vs 8.3%; difference, -6.5% [95% CI, -11.4% to -1.4%]) and wound complications (5.6% vs 16.0%; difference, -11.7% [95% CI, -18.6% to -4.6%]) were less common with robotic surgery than open surgery. Participants undergoing open surgery reported worse quality of life vs robotic surgery at 5 weeks (difference in mean European Quality of Life 5-Dimension, 5-Level instrument scores, -0.07 [95% CI, -0.11 to -0.03]; P = .003) and greater disability at 5 weeks (difference in World Health Organization Disability Assessment Schedule 2.0 scores, 0.48 [95% CI, 0.15-0.73]; P = .003) and at 12 weeks (difference in WHODAS 2.0 scores, 0.38 [95% CI, 0.09-0.68]; P = .01); the differences were not significant after 12 weeks. There were no statistically significant differences in cancer recurrence (29/161 [18%] vs 25/156 [16%] after robotic and open surgery, respectively) and overall mortality (23/161 [14.3%] vs 23/156 [14.7%]), respectively) at median follow-up of 18.4 months (IQR, 12.8-21.1).
Conclusions and relevance: Among patients with nonmetastatic bladder cancer undergoing radical cystectomy, treatment with robot-assisted radical cystectomy with intracorporeal urinary diversion vs open radical cystectomy resulted in a statistically significant increase in days alive and out of the hospital over 90 days. However, the clinical importance of these findings remains uncertain.
百度浏览 来源 : 医微客
版权声明:本网站所有注明来源“医微客”的文字、图片和音视频资料,版权均属于医微客所有,非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源:”医微客”。本网所有转载文章系出于传递更多信息之目的,且明确注明来源和作者,转载仅作观点分享,版权归原作者所有。不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。 本站拥有对此声明的最终解释权。



发表评论
注册或登后即可发表评论
登录注册
全部评论(0)